Sexually transmitted fungal infections (STFIs) are quickly rising to the forefront of sexual health discussions. Historically, the attention has focused on bacterial and viral infections, but now fungi like Candida and dermatophytes are becoming major players in this arena. This shift not only highlights an urgent need for education but also pushes healthcare providers to reconsider how they approach sexual health. The consequences of ignoring STFIs can be severe, as they pose unique risks that can complicate relationships and health outcomes.
The Rise of Sexually Transmitted Fungal Infections
The prevalence of sexually transmitted fungal infections has soared in recent years, largely due to multiple factors. Increased antibiotic use disrupts our microbiome, paving the way for fungi to thrive. In 2024, a study found that regions with high antibiotic consumption saw candidiasis rates spike by 30%. This unsettling trend points to a critical link between our medical practices and fungal health risks.
Moreover, today’s lifestyle habits contribute heavily to this issue. The modern diet, rife with sugars and processed foods, creates an environment where fungi can flourish. A 2025 health report indicated that changes in diet correlate with heightened candidiasis rates. This intersection of dietary habits and health priorities reinforces the importance of awareness and education in combating STFIs.
Compromised immune systems also play a role. Conditions like HIV, diabetes, and even the lingering effects of COVID-19 leave individuals vulnerable to infections that many might dismiss. As we witness a surge in these immune conditions, it becomes increasingly evident that sexually transmitted fungal infections are more than just a minor health issue; they’re a significant public health concern that warrants immediate attention.

5 Types of Sexually Transmitted Fungal Infections to Watch
Often referred to as a yeast infection, candidiasis is a primary example of sexually transmitted fungal infections. Triggered by factors such as antibiotic use, hormonal shifts, and weakened immunity, its transmission through sexual contact adds another layer of complexity. With statistics showing that high antibiotic usage increases the likelihood of candidiasis, this is a clear indication that medical practices have repercussions for sexual health.
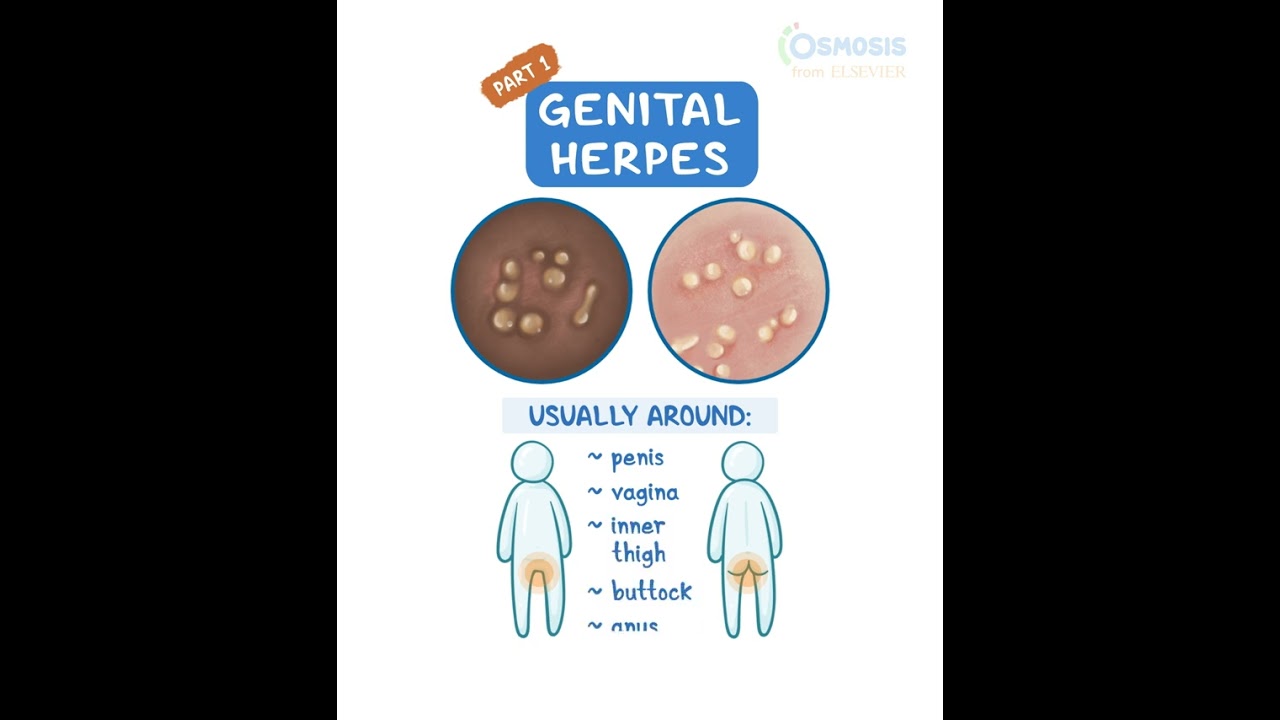
Commonly known as ringworm, dermatophyte infections can slip under the radar. Despite their common association with athletes, they can be transmitted through intimate contact. Tinea cruris, often mistaken for harmless skin irritations, has been reported by athletes participating in sports, emphasizing the need for vigilance in evaluating skin conditions during intimate moments.
This fungal infection primarily affects the respiratory system but can also emerge from intimate exposure in contaminated environments. Recent cases in 2023 illustrated how one partner’s exposure to polluted surroundings led to risks of infection in the relationship. As awareness grows, we see how environments, not just behaviors, can influence the spread of sexually transmitted fungal infections.
Typically inhaled through spores, histoplasmosis has found a novel transmission route among sexual partners. Close living quarters or shared environments contaminated with bird or bat droppings show new avenues of risk. Such instances are rarely discussed, yet they highlight the need for nuanced conversations around sexually transmitted fungal infections.
While not considered a traditional sexually transmitted disease, pityriasis versicolor can spread between partners via skin-to-skin contact. Characterized by patches of discolored skin, this condition reinforces that even conditions typically classified outside of STIs can have intimate transmission pathways.
Why Are Sexually Transmitted Fungal Infections Increasing?
The rise in sexually transmitted fungal infections can be traced back to several interlinked factors. First, the over-prescription of antibiotics has disrupted the body’s natural microbiota, allowing fungal organisms to multiply unchecked. A comprehensive look at health data reveals that individuals treated with antibiotics in the past six months are significantly more prone to candidiasis.
Secondly, we can’t overlook the impact of lifestyle. Increased sugar consumption leads to an environment that favors fungal growth. A 2025 report correlating dietary habits with health outcomes sheds light on how our modern lifestyle contributes to this alarming trend in sexual health.
Lastly, the prevalence of immunocompromised individuals is rising. Chronic conditions such as HIV or diabetes are becoming more common, making those affected more susceptible to every infection type, including fungal ones. This demographic shift raises serious questions about how we approach patient care and prevention strategies.

Managing Sexually Transmitted Fungal Infections
Addressing the challenge of sexually transmitted fungal infections requires a multifaceted approach. Key strategies involve education, lifestyle changes, and targeted medical treatments.
Education is crucial in raising awareness about symptoms and transmission. Effective health campaigns, especially targeting communities most at risk, can drastically lower infection rates. It’s about fostering understanding so individuals know how to protect themselves and their partners.
Lifestyle adjustments can also play a significant role in prevention. By promoting dietary changes, such as incorporating more probiotics, we can boost natural defenses against these infections. This strategy advocates for a return to more natural eating habits, steering clear of excessive sugars.
Targeted treatments are continuously evolving. Antifungal medications like fluconazole have advanced, offering broader coverage with fewer side effects. Ongoing research is crucial in developing new therapies to combat the rise of sexually transmitted fungal infections effectively.
The Future of Sexual Health and Fungal Infections
The recognition of sexually transmitted fungal infections as serious public health issues marks a shift in how we understand sexual health. Healthcare providers and public health authorities must prioritize education and research to manage these infections effectively. By enhancing awareness, we can drive innovation in both prevention and treatment.
Furthermore, as conversations around sexual health continue to evolve, it’s imperative for healthcare professionals, researchers, and individuals to participate in ongoing dialogues. Addressing sexually transmitted fungal infections through a collaborative approach will work towards a healthier future for everyone.
Ten years from now, we may look back and realize that recognizing the complexities posed by these infections was as essential as the battle against traditionally recognized STIs. The future of sexual health hinges on understanding how every aspect of our health, environment, and behavior intertwines. Let’s choose to be informed, proactive, and responsible about sexual health for a healthier tomorrow.
In an age where each factor—be it our environment or diet—contributes to health, we must remain vigilant. As we do so, the conversation around sexually transmitted fungal infections will shape the future dynamics of sexual health, ensuring we’re better equipped to handle the transitions ahead.
For more engaging content, check out how Starlight Glimmer exemplifies resilience here, or dive into the inspiring journey of Demet Özdemir here. Don’t miss the latest on films like Breakwater here. Looking to inspire young minds? Check out KidZania Cuicuilco here. For a dose of humorous understanding around unpredictable situations, explore Murphy’s Law here. Delve into music trends and find out when is Spotify Wrapped 2025 here. Feeling nostalgic? Check out the beloved classic A Charlie Brown Christmas here. If you’re a sports fanatic, explore the Los Angeles Rams vs. Chicago Bears match player stats here. Finally, discover how Talkie is changing the conversation here.
Fun Trivia About Sexually Transmitted Fungal Infections
The Unexpected Realities
Did you know that sexually transmitted fungal infections aren’t just a nuisance? They can actually lead to serious health issues if left untreated. For instance, candidiasis, often called a yeast infection, isn’t just a problem for women; men can be affected, too! Fungal infections in men can often go unnoticed( until they cause major discomfort.
Interestingly, the Candida fungus is part of our body’s normal flora. Yep, that means it’s lurking in your body right now! But under certain conditions, it can spin out of control, leading to infections. Stress, poor diet, and antibiotics can tip the balance, allowing this tiny foe to gain the upper hand. Signs of yeast infections can sometimes mimic other conditions( making diagnosis tricky!
Awareness and Prevention
While many folks think of STIs as solely bacterial or viral, sexually transmitted fungal infections deserve their time in the spotlight. One alarming fact: many STIs are passed on without showing symptoms. This makes education and awareness crucial for prevention. Knowledge is power, and understanding the different types of STIs( can save you from unnecessary health issues down the line.
Another fun tidbit: some sexually transmitted fungal infections can also spread via non-sexual contact. For example, sharing clothes or towels can lead to infection! So, when you’re out having fun, be mindful of your surroundings and personal items. Hygiene isn’t just a buzzword—it’s a lifestyle!
Getting Comfortable with the Uncomfortable
Facing the reality of sexually transmitted fungal infections is vital, yet it can feel a bit awkward. However, tackling these infections head-on can prevent even bigger issues later. Understanding how to effectively treat infections( is just as important as knowing how to prevent them. So, whether you’re single or in a relationship, be proactive about your sexual health—after all, it’s a shared responsibility!
Lastly, don’t forget about the power of communication. Talking to your partner about sexual health can feel uncomfortable, but it’s key to maintaining a healthy relationship. Let’s face it: the more knowledge and openness, the better prepared you both will be to navigate those pesky sexually transmitted fungal infections.
What is the new sexually transmitted fungus?
The new sexually transmitted fungus is Candida auris, which has raised concern due to its resistance to treatment and the potential for outbreaks in healthcare settings.
Can a woman give a man a fungal infection?
Yes, a woman can pass a fungal infection to a man, although it’s more common for men to contract fungal infections from women via sexual contact.
Are fungi sexually transmissible?
Fungi can indeed be sexually transmissible, especially certain strains like Candida that can be passed during intimate contact.
Can sperm carry fungal infections?
Sperm itself doesn’t carry fungal infections, but if a man has a fungal infection, it’s possible for the infection to be present in bodily fluids during sexual activity.
What STD is caused by a fungus?
An STD caused by a fungus is candidiasis, commonly known as a yeast infection, which can affect both men and women.
What are the four new STDs?
The four new STDs that are emerging include Mycoplasma genitalium, Trichomoniasis, Toxoplasmosis, and the recently identified fungal STDs like Candida auris.
How does a man know if he has a fungal infection?
A man might suspect he has a fungal infection if he experiences symptoms like itching, redness, or unusual discharge in the genital area.
Can my boyfriend give me fungus if they bave fungus on their feet?
Yes, if your boyfriend has a fungal infection on his feet, it’s possible for him to transfer it to you through skin-to-skin contact, although it’s not very common.
Can yeast infections be caused by a cheating partner?
Yeast infections aren’t directly caused by a partner cheating, but exposure to new partners could potentially introduce different bacteria or fungi that disrupt the natural balance.
What are five diseases caused by fungi?
Five diseases caused by fungi include ringworm, athlete’s foot, thrush, histoplasmosis, and Aspergillosis, each varying in severity and symptoms.
Is fungus highly contagious?
Fungus can be contagious, especially in warm, moist environments, and through direct contact, but it doesn’t spread as easily as some bacteria or viruses.
What is the first sexually transmitted fungal infection?
The first sexually transmitted fungal infection identified is Candida auris, which has highlighted the need for awareness and prevention in sexual health.
How to remove fungus from private parts?
To remove fungus from private parts, it’s best to keep the area clean and dry, use antifungal creams or medications as prescribed, and avoid irritants like scented soaps.
What is the new fungal STD?
The new fungal STD refers to Candida auris, which poses treatment challenges and can lead to serious health issues if not addressed quickly.
Why is your sperm yellow?
Yellow sperm can be due to several reasons, including the presence of infections, dietary factors, or even dehydration, but if it’s persistent, it’s worth checking out with a healthcare professional.
What are the symptoms of the new fungus virus?
Symptoms of the new fungus virus include itching, unusual discharge, and irritation, similar to those seen with common yeast infections.
What is the new sexually transmitted disease going around?
The new sexually transmitted disease currently gaining attention is linked to Candida auris, raising concerns about fungal infections in sexual health discussions.
How to remove fungus from private parts?
To remove fungus from private parts, maintain cleanliness, use prescribed antifungals, wear breathable underwear, and avoid moisture buildup.
What is the new superbug fungus?
The new superbug fungus refers to Candida auris, which is resistant to many antifungal treatments and has become a major public health concern.